Introduction
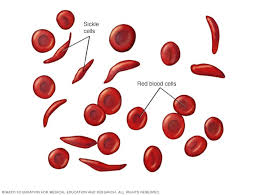
- Sickle cell anemia ek genetic blood disorder hai jisme red blood cells (RBCs) ka shape abnormal ho jata hai.
- Normal RBCs gol aur flexible hote hain, lekin sickle cell anemia mein yeh cells crescent (advi) ya sickle shape mein badal jaate hain.
- Yeh problem hoti hai hemoglobin S (HbS) ki wajah se, jo RBCs mein hota hai.
- Yeh sickle-shaped cells blood vessels ke through properly nahi nikal paate, jiski wajah se blood flow block ho jata hai, aur pain aur organ damage ho sakta hai.
- Yeh ek inherited disease hai, matlab yeh apne parents se milti hai.
- Sickle cell anemia zyada tar un logon mein hota hai jo African, Mediterranean, Middle Eastern, aur Indian descent se hote hain.
- Sickle cell anemia ka koi permanent cure nahi hai, lekin proper treatment aur care se iske symptoms manage kiye jaa sakte hain aur affected individuals apni life ache se jee sakte hain.
Etiology
Sickle cell anemia ka main cause ek genetic mutation hai. Yeh mutation us gene mein hota hai jo hemoglobin banane ke liye responsible hota hai. Is mutation ke karan, hemoglobin S (HbS) banne lagta hai, jo normal hemoglobin A (HbA) se alag hota hai. Jab hemoglobin S oxygen lose karta hai, toh yeh stick karna shuru ho jata hai aur RBCs mein long, stiff rods ban jate hain. Yeh rods RBCs ko sickle shape de dete hain, jisse cells rigid aur sticky ho jaate hain.
-
Inheritance Pattern:
-
Sickle cell anemia ek autosomal recessive pattern mein inherit hoti hai.
-
Iska matlab hai ki agar kisi ko yeh disease honi hai, toh unhe apne dono parents se sickle cell gene milna zaroori hai.
-
Agar kisi ko sirf ek sickle cell gene milta hai, toh unhe sickle cell trait hota hai.
-
Sickle cell trait wale log symptoms nahi dikhate, lekin yeh gene agle generation ko pass kar sakte hain.
-
-
Co-inheritance of Other Genes:
-
Kabhi-kabhi sickle cell anemia ke saath dusre genetic disorders bhi ho sakte hain, jaise thalassemia, jo iske symptoms ko aur complex bana sakte hain.
-
Epidemiology
Sickle cell anemia duniya bhar mein millions of logon ko affect karti hai. Yeh disorder un regions mein zyada hoti hai jahan malaria ka risk zyada hota hai. Yeh isliye hota hai kyunki sickle cell trait se log malaria se protect ho jaate hain.
-
Sub-Saharan Africa: Yeh region sabse zyada affected hai. U.S. mein lagbhag 1 in 365 African American babies ko sickle cell anemia hoti hai.
-
Middle East, Mediterranean, aur India: Yeh regions mein bhi cases hain, lekin Africa ke mukable thode kam hain. Mediterranean ya Indian descent wale logon mein bhi sickle cell disease ho sakti hai.
-
Worldwide: Har saal lagbhag 3 lakh bachche sickle cell anemia se paida hote hain. U.S. mein yeh disease zyada tar African Americans ko hoti hai, lekin yeh Hispanics, Mediterranean, aur Middle Eastern backgrounds wale logon mein bhi dekhi jaati hai.
Pathophysiology
Sickle cell anemia ka pathophysiology matlab hai uss mechanism ko samajhna jisme body mein problem hoti hai. Yeh disease RBCs ke behaviour se related hai.
-
Sickle Cell Formation: Jab blood mein oxygen kam hota hai, toh hemoglobin S ek dusre ke saath chipakne lagta hai. Isse RBCs sickle shape mein badal jaati hain. Yeh sickle cells blood vessels ke through asaani se nahi nikal paate aur blood flow block kar dete hain.
-
Hemolysis (RBCs ka tootna): Normal RBCs ka lifespan 120 din hota hai, lekin sickle cells jaldi toot jaate hain. Yeh premature destruction anemia (kam RBCs) ki wajah banta hai.
-
Vaso-occlusion (Blood Flow ka rukna): Sickle cells blood vessels ko block kar sakte hain, jisse oxygen ki supply kam ho jaati hai. Yeh pain crises ko trigger karte hain aur organs ko damage karte hain. Jab blood flow rukta hai, toh organs jaise brain, kidneys, aur lungs damage ho sakte hain.
-
Inflammation (Sojaav): Sickle cells blood vessels mein inflammation kar sakte hain, jo aur zyada blockage aur tissue damage ka reason ban sakti hai. Time ke saath yeh blood vessels ko stiff bana deti hai, jo repair ko mushkil bana deti hai.
-
Organ Damage: Chronic pain, blood flow ka rukna, aur organ damage se long-term issues ho sakte hain. Spleen jo blood filter karta hai, woh damage ho sakta hai (isko autosplenectomy kehte hain). Isse body infections se jyada vulnerable ho jaati hai.
Laboratory Investigations
Laboratory investigations sickle cell anemia ko diagnose karne, uski progression ko monitor karne, aur complications ko evaluate karne ke liye zaroori hoti hain. Yeh tests doctors ko disease ki severity samajhne mein madad karte hain aur treatment decisions lene mein guide karte hain. Yahan par sabse common tests diye gaye hain jo sickle cell anemia ko diagnose aur manage karne ke liye use kiye jaate hain:
Complete Blood Count (CBC)
Complete Blood Count (CBC) ek basic aur important test hai jo kisi bhi blood disorder ko assess karne ke liye kiya jata hai, including sickle cell anemia.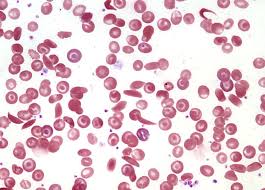
-
Red Blood Cell (RBC) Count: Sickle cell anemia mein RBC count kam hota hai, kyunki sickle cells ka premature destruction hota hai (hemolysis). Isse anemia ho jaati hai, matlab blood mein healthy RBCs ki kami hoti hai, jo oxygen ko properly carry kar sakein.
-
Reticulocyte Count: Yeh test bone marrow mein nayi red blood cells ki production ko measure karta hai. Sickle cell anemia mein reticulocyte count usually high hota hai, kyunki body sickle cells ke destruction ko compensate karne ke liye zyada RBCs bana rahi hoti hai.
-
Hemoglobin Level: Sickle cell anemia mein hemoglobin ka level kam hota hai, jo anemia ko worsen karta hai.
-
White Blood Cell (WBC) Count: Kabhi-kabhi WBC count thoda high bhi ho sakta hai, especially jab pain crises ya infection ho, kyunki body stress aur inflammation respond karti hai.
-
Platelet Count: Platelets bhi elevated ho sakte hain sickle cell anemia mein, kyunki inflammation aur tissue damage zyada hota hai.
Peripheral Blood Smear
Peripheral blood smear ek aisa test hai jisme blood sample ko slide par spread karke microscope se dekha jaata hai. Yeh test sickle cell anemia ko diagnose karne mein madad karta hai.
-
Sickle-Shaped Cells: Blood smear par sabse pehli cheez jo dikhti hai, woh hai sickle-shaped RBCs. Yeh cells crescent (advi) shape ke hote hain, jo round aur flexible nahi hote, aur inhe blood vessels se nikalne mein problem hoti hai.
-
Target Cells: Target cells bhi dikh sakte hain, jo RBCs mein ek dark center aur ek lighter ring bana dete hain. Yeh abnormal cells sickle cell anemia mein common hote hain.
-
Howell-Jolly Bodies: Yeh RBCs ke andar ke nucleus ke remnants hote hain, jo spleen ke damage hone ka indication dete hain. Sickle cell disease mein spleen damage ho jata hai.
-
Nucleated Red Blood Cells: Kabhi-kabhi nucleated RBCs bhi dikh sakte hain, jo sign hai ki bone marrow rapidly RBCs bana raha hai.
Hemoglobin Electrophoresis
Hemoglobin electrophoresis ek test hai jo blood mein different types of hemoglobin ko identify karta hai. Yeh test sickle cell anemia ko confirm karne ke liye sabse accurate aur important hai.
-
Hemoglobin S (HbS): Sickle cell anemia mein HbS ka amount zyada hota hai. Is test mein agar sickle cell anemia hai, toh mostly hemoglobin S dikhai dega aur hemoglobin A (normal hemoglobin) nahi dikhai dega.
-
Hemoglobin F (HbF): Kuch logon mein, particularly jinhe hydroxyurea treatment diya gaya ho, fetal hemoglobin (HbF) ka level zyada ho sakta hai. HbF sickling ko reduce karta hai aur pain crises ko kam karta hai.
-
Hemoglobin A: Sickle cell anemia mein, hemoglobin A bilkul nahi dikhai deta, lekin agar koi person sickle cell trait (carrier) hai, toh unme HbS aur HbA dono hote hain, jisme HbA zyada hota hai.
-
Other Abnormal Hemoglobins: Agar koi dusri hemoglobinopathy bhi hai, jaise hemoglobin C ya SC disease, toh woh bhi is test ke through identify ki jaa sakti hai.
Sickle Cell Solubility Test
Sickle cell solubility test ek screening test hai jo hemoglobin S (HbS) ki presence ko detect karta hai. Yeh test jaldi aur asaan hai, lekin hemoglobin electrophoresis se kam specific hota hai.
-
Yeh test blood sample mein ek reagent add karke hota hai, jisse hemoglobin S oxygen ke low levels par precipitate (solid clump) ho jata hai. Agar sickle hemoglobin hai, toh solution clouded (turbid) ho jaata hai, jo positive result ko indicate karta hai.
-
Yeh test sickle cell anemia aur sickle cell trait (carrier) ke beech differentiate nahi kar sakta, isliye iske baad usually hemoglobin electrophoresis ki zaroorat hoti hai.
Reticulocyte Count
Reticulocyte cot test bone marrow ke RBC production ko measure karta hai, jo sickle cell anemia mein elevated hota hai.
-
Increased Reticulocytes: Agar reticulocyte count zyada ho, toh iska matlab hai ki body sickle cells ke loss ko compensate karne ke liye nayi RBCs produce kar rahi hai. Yeh zyada tar hemolytic crisis (jab RBCs zyada toot rahe hote hain) mein dekha jaata hai.
-
Chronic Anemia: Sickle cell anemia chronic anemia hai, isliye despite increased reticulocytes, total RBC count low hi rehta hai.
Lactate Dehydrogenase (LDH) and Bilirubin Levels
Lactate Dehydrogenase (LDH) aur bilirubin levels ko monitor karte hain taaki RBC destruction (hemolysis) ki extent ko samjha ja sake.
-
LDH: LDH ek enzyme hai jo RBCs mein hota hai. Jab RBCs toot te hain, toh LDH bloodstream mein release ho jata hai. Agar LDH levels high hain, toh yeh indicate karta hai ki hemolysis ho raha hai aur organs damage ho rahe hain, jaise liver ya kidneys.
-
Bilirubin: Bilirubin RBCs ke breakdown se banta hai. Agar hemolysis zyada ho, toh bilirubin levels high ho jaate hain, jo unconjugated bilirubin ko increase karte hain, aur isse jaundice (skin aur eyes ka yellow hona) ho sakta hai. Sickle cell anemia mein chronic hemolysis ki wajah se mild jaundice ka hona common hai.
Doppler Ultrasound and MRI
Doppler ultrasound aur MRI imaging techniques hain jo sickle cell anemia ke complications ko monitor karte hain, especially brain aur organs ke issues ko.
-
Doppler Ultrasound of the Cerebral Arteries: Sickle cell anemia ke bachon mein, Doppler ultrasound se brain ki major arteries ka blood flow check kiya jaata hai. Yeh test stroke aur cerebrovascular disease ke early signs ko detect karne mein madad karta hai. Regular Doppler ultrasound se doctors high-risk patients ko identify kar sakte hain aur unhe early intervention de sakte hain.
-
MRI of the Brain: MRI silent strokes (aise strokes jo symptoms nahi dikhate) aur brain ke dusre abnormalities ko detect karne mein madad karta hai. Yeh brain ko monitor karne ka useful tool hai, jisse stroke ke effects ko track kiya jaa sakta hai.
-
MRI of Other Organs: MRI ko other organs jaise liver, spleen, aur kidneys ke damage ko assess karne ke liye bhi use kiya jaata hai.
Chest X-Ray
Chest X-ray ek imaging test hai jo respiratory complications ko detect karta hai, jo sickle cell anemia mein common hoti hain, jaise acute chest syndrome.
-
Acute Chest Syndrome: Yeh sickle cell anemia ka life-threatening complication hota hai, jo lung tissue damage ki wajah se hota hai. Chest X-ray mein lung consolidation dikhai de sakta hai, jo pneumonia ya infarction (tissue death due to lack of blood flow) ka sign hota hai.
-
Other Lung Abnormalities: Chronic lung damage ko bhi chest X-ray se dekha jaa sakta hai, jo sickle cell anemia mein common hai.
Treatment and Management
Sickle cell anemia ka treatment symptoms ko manage karne aur complications ko prevent karne par focus karta hai.
-
Pain Management: Pain crises ko treat karna zaroori hota hai. Iske liye:
-
Pain medications: Opioids aur NSAIDs (non-steroidal anti-inflammatory drugs) diye jaate hain.
-
Hydration: Pani peena zaroori hai, kyunki dehydration se cells zyada sickle ho sakte hain.
-
Oxygen therapy: Low oxygen levels ke time oxygen diya jata hai, jo sickling ko reduce karta hai.
-
-
Blood Transfusions: Agar symptoms severe hain, toh blood transfusions diye jaate hain, jisse sickle cells ko normal RBCs se replace kiya jaata hai.
-
Hydroxyurea: Yeh medicine fetal hemoglobin (HbF) ko increase karti hai, jo sickling ko reduce karta hai. Hydroxyurea pain crises ko reduce karta hai aur blood transfusions ki zaroorat ko kam karta hai.
-
Bone Marrow or Stem Cell Transplantation: Bone marrow transplant ek possible cure ho sakta hai, lekin yeh complex aur risky hota hai.
-
Antibiotics aur Vaccinations: Sickle cell anemia wale log infections ke liye jyada vulnerable hote hain. Vaccinations aur penicillin jaisi antibiotics diye jaate hain.
-
Gene Therapy: Gene therapy ek promising treatment hai jisme genetic defect ko thik kiya jaata hai, lekin yeh abhi bhi research mein hai.
Management
Sickle cell anemia ka management complications ko prevent karne aur symptoms ko control karne ke liye zaroori hota hai:
-
Prevention of Complications: Regular doctor visits aur timely treatment se complications jese stroke, kidney damage, aur organ failure ko roka jaa sakta hai.
-
Psychosocial Support: Chronic pain aur uncertain future ko handle karna emotionally challenging hota hai. Counseling aur mental health support zaroori hai.
-
Education: Patients aur caregivers ko sickle cell ke baare mein educate karna zaroori hai, jaise pain crises ko pehchanna, hydration ka importance, aur jab medical help chahiye ho.
-
Prenatal Screening: Agar family mein sickle cell ka history ho, toh genetic counseling aur prenatal testing ki madad se yeh jaancha jaa sakta hai ki future children ko yeh disease ho sakti hai ya nahi.