Introduction
- Thalassemia ek genetic blood disorder hai, jisme body mein hemoglobin ka production kam ya bilkul nahi hota.
- Hemoglobin ek protein hai jo red blood cells mein hota hai aur oxygen body ke alag-alag parts tak pahuchata hai.
- Jab thalassemia hoti hai, toh ya toh alpha-globin ya beta-globin chains ka production kam ho jata hai, jo thalassemia ke type par depend karta hai.
-
Alpha-thalassemia mein alpha-globin chains ka production kam hota hai.
-
Beta-thalassemia mein beta-globin chains ka production kam hota hai.
- Is condition ke do major types hote hain: thalassemia minor (carrier status, jo mild symptoms ke saath hota hai) aur thalassemia major (severe form jo intensive medical care ki zarurat hoti hai).

Aetiology
Thalassemia ka cause hai genetic mutations jo alpha-globin aur beta-globin genes mein hoti hai.
-
Alpha-Thalassemia:
-
Ye HBA1 aur HBA2 genes mein deletion ya mutation ki wajah se hota hai, jo chromosome 16 par located hain aur jo alpha-globin chains banate hain.
-
Alpha-thalassemia trait (carriers) mein ek defective gene hota hai, jo usually mild anemia ya bilkul bhi symptoms nahi deta.
-
Alpha-thalassemia major (hydrops fetalis) jab hota hai jab 4 alpha-globin genes defective hote hain, aur ye condition fetus mein hi fatal ho sakti hai.
-
-
Beta-Thalassemia:
-
Ye HBB gene mein mutation ki wajah se hota hai, jo chromosome 11 par hota hai aur jo beta-globin chains banata hai.
-
Beta-thalassemia minor (thalassemia trait) ek defective beta-globin gene hone se hota hai, jisme mild anemia hota hai.
-
Beta-thalassemia major (Cooley’s anemia) tab hota hai jab do defective beta-globin genes inherit hote hain, aur yeh severe anemia cause karta hai, jisme regular blood transfusions ki zarurat hoti hai.
-
Inheritance ka pattern autosomal recessive hota hai, iska matlab hai ki agar dono parents mein se koi ek carrier hai, toh unka baccha thalassemia ka carrier ho sakta hai, lekin disease tabhi hovegi jab dono parents se defective gene milta hai.
Epidemiology
Thalassemia duniya ke kai regions mein common hai, aur kuch specific regions mein iska prevalence zyada hai:
-
Geographic Distribution:
-
Beta-thalassemia Mediterranean countries (jaise Greece, Italy, Arabs) mein common hai. Yeh South Asia, Southeast Asia, aur North Africa mein bhi zyada hota hai.
-
Alpha-thalassemia mainly Southeast Asia, China, aur Africa mein hota hai.
-
Countries like India, Pakistan, Bangladesh, Thailand, aur China mein thalassemia kaafi zyada hai. Yeh regions mein lagbhag 5-7% log thalassemia gene ke carrier hote hain.
-
-
Global Prevalence:
-
Thalassemia ek common genetic disorder hai, aur duniya bhar mein millions of carriers aur affected individuals hain.
-
Thalassemia major usually early childhood mein manifest hota hai aur isse kai health complications ho sakti hain.
-
-
Carrier Status:
-
Lagbhag 5% global population mein thalassemia gene ka carrier status hota hai, jo unhone kabhi notice nahi kiya hota kyunki carriers ko usually mild ya koi symptoms nahi hote.
-
-
Impact on Healthcare:
-
High prevalence wale regions mein thalassemia health systems par kaafi burden dalti hai, especially blood transfusions aur iron chelation therapy ke liye.
-
Pathophysiology
Thalassemia ka pathophysiology kaafi complex hai, aur do main processes involve hoti hain: ineffective erythropoiesis (red blood cell production ka ineffective hona) aur hemolysis (red blood cells ka premature destruction).
-
Imbalanced Hemoglobin Production:
-
Normal hemoglobin mein do alpha-globin aur do beta-globin chains hoti hain. Thalassemia mein, ek type ki globin chain (alpha ya beta) ka production kam ya absent hota hai.
-
Beta-thalassemia mein beta-globin chains ka production kam ya absent hota hai, aur alpha-globin chains ka production normal ya zyada hota hai.
-
Alpha-thalassemia mein alpha-globin chains ka production kam ya absent hota hai, aur isse beta-globin chains ka excess production hota hai.
-
-
Excess Unpaired Chains:
-
Jo globin chains (alpha ya beta) zyada produce hoti hain, wo unstable hoti hain aur red blood cells ke andar precipitate ho jati hain. Yeh red blood cells ko damage karte hain aur unka premature destruction (hemolysis) hota hai.
-
-
Bone Marrow Expansion:
-
Body anemia ko compensate karne ke liye bone marrow mein red blood cell production badhane ki koshish karti hai, jiske wajah se marrow expand hota hai aur skeletal deformities (jaise “chipmunk facies”) hoti hain.
-
-
Iron Overload:
-
Frequent blood transfusions ke wajah se iron ka excess body mein accumulate ho jata hai, jo liver, heart aur endocrine glands mein deposit hota hai aur iron overload ka cause banta hai. Isse liver failure, heart failure, aur diabetes ho sakte hain.
-
Laboratory Investigations
Thalassemia ka diagnosis aur monitoring kai laboratory tests se kiya jata hai: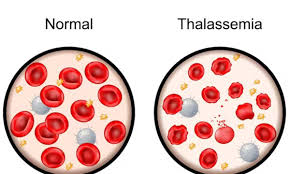
-
Complete Blood Count (CBC):
-
Microcytic hypochromic anemia: Red blood cells ka size chhota hota hai (low mean corpuscular volume, MCV) aur unme color pale hota hai (low mean corpuscular hemoglobin, MCH).
-
Low hemoglobin (Hb) levels.
-
Increased reticulocyte count jisse bone marrow response dikhata hai.
-
-
Peripheral Blood Smear:
-
Target cells: Red blood cells jo dark center aur ring jaisi appearance dikhate hain.
-
Nucleated red blood cells: Immature red blood cells jo blood mein dikhte hain.
-
Anisopoikilocytosis: Red blood cells ka size aur shape ka variation.
-
-
Hemoglobin Electrophoresis:
-
Ye test important hai thalassemia diagnose karne ke liye.
-
Beta-thalassemia mein HbA2 aur HbF levels zyada hote hain.
-
Alpha-thalassemia mein electrophoresis normal hota hai.
-
-
Genetic Testing:
-
DNA analysis se specific mutations ka pata chal sakta hai jo HBA1, HBA2, aur HBB genes mein hoti hain.
-
-
Iron Studies (Serum Ferritin, Serum Iron, Transferrin Saturation):
-
Ye tests iron overload ko monitor karne ke liye hote hain.
-
-
Liver Function Tests:
-
Liver mein iron accumulation ke effect ko assess karne ke liye.
-
-
*MRI (T2 for Iron Overload)**:
-
Iron overload ko monitor karne ke liye liver aur heart MRI ki jaati hai.
-
Management
Thalassemia ka treatment symptoms ko control karne, complications ko prevent karne aur life quality improve karne ke liye hota hai. Treatment ka approach disease ke severity par depend karta hai.
-
General Measures:
-
Folic acid supplements red blood cell production ko support karte hain.
-
Regular monitoring zaruri hoti hai hemoglobin levels, iron status aur organ function ke liye.
-
-
Blood Transfusions:
-
Thalassemia major ke liye blood transfusions important hote hain. Yeh transfusions regular interval par diye jaate hain, taaki hemoglobin levels maintain ho sakein.
-
-
Iron Chelation Therapy:
-
Frequent transfusions se body mein iron ka excess accumulation hota hai, jise iron chelation therapy se remove karna padta hai.
-
Common chelators hain:
-
Deferoxamine (intravenous ya subcutaneous).
-
Deferasirox aur Deferiprone (oral chelators).
-
-
-
Bone Marrow/Stem Cell Transplantation:
-
Curative treatment bone marrow transplant hai, jo agar jaldi hota hai toh bacha ke life ko bacha sakta hai.
-
-
Gene Therapy:
-
Gene therapy ek promising approach hai, jisme thalassemia ke defective gene ko correct karne ki koshish ki ja rahi hai.
-
-
Splenectomy:
-
Agar spleen enlarge ho jati hai aur hypersplenism (blood cells ka excessive destruction) ho raha hai, toh splenectomy ki ja sakti hai.
-
-
Prenatal Diagnosis and Genetic Counselling:
-
Prenatal genetic testing (amniocentesis ya chorionic villus sampling) se fetus mein thalassemia detect kiya ja sakta hai, jisse parents informed decisions le sakte hain.
-