Introduction
- Hemolytic Disease of the Newborn (HDN) ek condition hai jo tab hoti hai jab maa aur baby ke khoon mein incompatibility hoti hai, jisse baby ke red blood cells (RBCs) ki destruction hoti hai (hemolysis).
- Yeh condition zyada tar Rh incompatibility se hoti hai, lekin ABO incompatibility ya other minor blood group incompatibilities ki wajah se bhi ho sakti hai.
- Red blood cells ke tootne se jo bilirubin banta hai, woh newborn ke khoon mein jama ho jata hai, jisse jaundice ho sakta hai aur agar treatment nahi kiya jaye toh aur bhi severe complications ho sakti hain jaise anemia, organ damage, ya fetal death.
Signs and Symptoms
HDN ke symptoms ki severity baby ki hemolysis (RBC destruction) ki degree aur diagnosis aur treatment ke time par depend karti hai. Common symptoms mein shamil hain:
-
Jaundice: Yeh ek hallmark sign hai HDN ka. Baby ka skin aur eyes yellow ho jate hain due to high bilirubin levels, jo RBCs ke tootne se banta hai. Jaundice usually pehle 24-48 hours ke andar develop hota hai.
-
Anemia: RBCs ki destruction ke wajah se baby ko pale hone, fatigue, aur weakness ho sakti hai. Severe anemia ke case mein baby ko lethargy, poor feeding, aur difficulty breathing bhi ho sakti hai.
-
Hepatosplenomegaly: Liver aur spleen badh jate hain kyunki body RBC destruction ko compensate karne ki koshish karti hai. Extreme cases mein yeh organ enlargement abdominal swelling ka karan ban sakta hai.
-
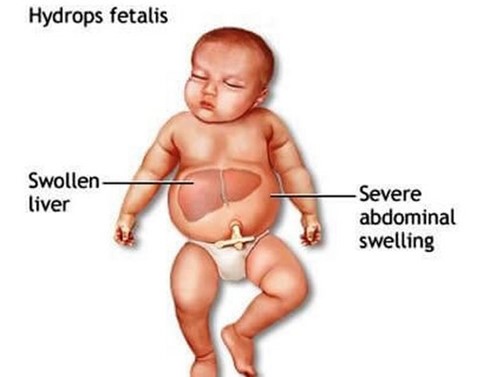
Edema (Hydrops fetalis): Yeh HDN ka ek severe form hai, jisme baby ka body poore tarah se swell ho jata hai, jaise abdomen, face, arms, legs, aur lungs ke aas-paas fluid ka accumulation. Agar treat nahi kiya jaye toh yeh fatal ho sakta hai.
-
Respiratory Distress: Severe anemia ke wajah se baby ko respiratory distress ho sakta hai, jisme baby ko oxygen milne mein mushkil hoti hai. Is condition mein baby ko oxygen support ki zarurat ho sakti hai.
-
Feeding Difficulties: HDN wale babies ko poor feeding habits ho sakti hain, kyunki woh general discomfort mehsoos karte hain ya phir anemia ya jaundice ki wajah se uncomfortable feel karte hain.
-
Abnormal Heart Rate: Agar anemia severe ho, toh baby ka heart rate abnormal ho sakta hai, jisme rapid heartbeat ya irregular heartbeat dekhne ko mil sakta hai.
Complications
HDN ke kuch severe complications ho sakte hain, jo agar untreated rahe toh permanent damage ka karan ban sakte hain:
-
Kernicterus: Yeh ek type ka brain damage hota hai jo excessive bilirubin ke wajah se hota hai. Yeh cerebral palsy, deafness, vision problems, aur cognitive impairment jaise long-term neurological deficits ka reason ban sakta hai. Yeh tab hota hai jab bilirubin levels dangerously high ho jaate hain aur brain tak pahunch jaate hain.
-
Severe Anemia: Agar treatment na kiya jaye toh HDN baby mein severe anemia ka karan ban sakta hai, jo blood transfusions ki zarurat pad sakti hai.
-
Hydrops Fetalis: Yeh HDN ka sabse severe form hai, jisme baby ke body mein fluid ka excessive accumulation hota hai, aur agar untreated rahe, toh fetal death ho sakta hai.
-
Organ Failure: RBCs ki overproduction ki wajah se liver, spleen aur heart enlarge ho jaate hain. Agar yeh organs apna function achhe se nahi kar paate, toh organ failure ho sakta hai, jisse aur complications ho sakti hain.
-
Premature Birth: Severe HDN ke case mein premature labor ho sakta hai, jo hydrops fetalis, severe anemia, ya intrauterine distress ki wajah se ho sakta hai.
Pathophysiology
HDN usually blood type incompatibility ki wajah se hota hai. Jab maa aur baby ke blood type match nahi karte, toh maa ka immune system baby ke red blood cells ko foreign samajhkar attack karta hai. Yeh attack red blood cells ke destruction (hemolysis) tak le jata hai. Do major mechanisms hain is condition ke hone ke: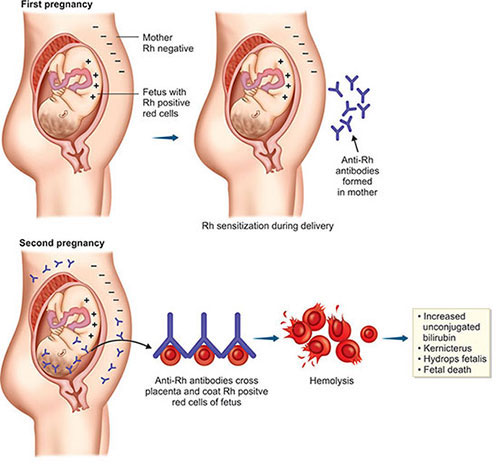
-
Rh Incompatibility:
-
Jab Rh-negative maa ke Rh-positive baby ke saath pregnancy hoti hai.
-
Pregnancy ya delivery ke time baby ka Rh-positive blood maa ke blood mein enter kar jata hai, aur maa ka immune system anti-Rh antibodies produce karta hai.
-
Yeh antibodies placenta se baby ke blood mein transfer ho jaati hain, aur baby ke red blood cells ko attack karke hemolysis karti hain.
-
-
ABO Incompatibility:
-
Yeh tab hota hai jab maa ka blood type O ho aur baby ka blood type A, B, ya AB ho.
-
Type O maa ka immune system naturally anti-A aur anti-B antibodies produce karta hai, jo baby ke red blood cells ko attack karte hain agar baby ka blood type A, B, ya AB ho.
-
-
Other Blood Group Incompatibilities:
-
Kell, Duffy, MNS antigens jaise minor blood group incompatibilities bhi HDN ka cause ban sakte hain, lekin yeh kaafi rare hote hain.
-
Serological Types of Hemolytic Disease of the Newborn
-
Rh Incompatibility:
-
Jab maa Rh-negative hoti hai aur baby Rh-positive hota hai.
-
-
ABO Incompatibility:
-
Jab maa ka blood type O ho aur baby ka blood type A, B, ya AB ho.
-
-
Other Minor Blood Group Incompatibilities:
-
Jaise Kell, Duffy, MNS antigens ke saath incompatibilities.
-
Diagnosis
HDN diagnose karne ke liye kai tests kiye jaate hain:
-
Maternal Blood Tests:
-
Antibody screening jo maa ke blood mein Rh antibodies ko check karta hai.
-
Blood typing jo maa aur baby ke blood types ko determine karta hai.
-
-
Newborn Blood Tests:
-
Bilirubin levels: Jaundice aur kernicterus ke risk ko monitor karta hai.
-
Complete blood count (CBC): Baby ke anemia aur red blood cell count ko assess karta hai.
-
Direct Coombs test: Yeh test baby ke RBCs par antibodies ko check karta hai. Positive Coombs test HDN ko indicate karta hai.
-
-
Ultrasound:
-
Agar hydrops fetalis ya organ involvement ka suspicion ho, toh ultrasound se baby ka condition assess kiya jata hai.
-
-
Amniocentesis:
-
Kuch cases mein amniotic fluid bilirubin levels ko measure kiya jata hai taaki condition ke severity ko assess kiya ja sake.
-
Prevention 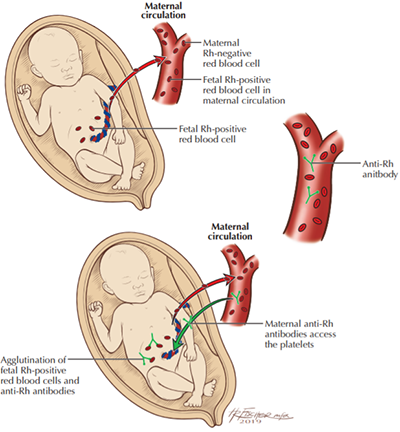
-
Rh Immunoglobulin (RhIg):
-
RhoGAM ya kisi aur Rh immunoglobulin ko Rh-negative mothers ko 28 weeks of pregnancy aur delivery ke baad diya jata hai agar baby Rh-positive ho. Yeh immune system ko Rh antibodies banne se rokta hai.
-
-
Early Blood Type Screening:
-
Pregnancy ke shuru mein blood type testing se at-risk pregnancies ka pata chal jata hai.
-
-
ABO Incompatibility:
-
ABO incompatibility ko prevent karna mushkil hai, lekin early detection aur treatment se condition ke effects ko kam kiya ja sakta hai.
-
After Birth Testing
Baby ke birth ke baad kuch tests kiye jaate hain:
-
Bilirubin levels: Jaundice aur kernicterus ke risk ko monitor karne ke liye.
-
Complete Blood Count (CBC): Anemia ko check karne ke liye.
-
Direct Coombs test: Baby ke RBCs par antibodies ko check karne ke liye.
Treatment
-
Phototherapy:
-
Blue light therapy ka use karke bilirubin ko break down kiya jata hai aur jaundice ko reduce kiya jata hai.
-
-
Exchange Transfusion:
-
Severe cases mein exchange transfusion ki zarurat padti hai jisme baby ka blood donor blood se replace kiya jata hai taaki bilirubin aur antibodies ko remove kiya ja sake.
-
-
Blood Transfusion:
-
Severe anemia ke cases mein blood transfusion ki zarurat hoti hai.
-
-
Supportive Care:
-
Yeh feeding support, intravenous fluids, aur oxygen therapy ko include karta hai.
-
Transfusion Reactions
Blood transfusion reactions mein shamil hain:
-
Fever
-
Chills
-
Rash
-
Back pain
-
Shortness of breath
Yeh reactions careful matching aur monitoring ke through minimize kiye jaate hain.
Epidemiology
-
Rh Incompatibility: Rh incompatibility ka prevalence region ke hisaab se vary karta hai. Lekin Rh immunoglobulin ka use karne ke baad Rh-related HDN ka incidence kaafi kam ho gaya hai.
-
ABO Incompatibility: ABO incompatibility zyada common hai aur lagbhag 15-20% pregnancies ko affect karta hai. Yeh usually less severe hota hai lekin still jaundice aur dusre complications cause kar sakta hai newborns mein.